Stomach Acid is Good for You!
If you have been watching television in the past decade you have seen the commercials. People suffering from heartburn and indigestion are magically cured by taking a little purple pill that combats the evil effects of stomach acid. No need to change your diet or other habits. Just pop a pill and everything will be ok. Just don’t pay too much attention to the list of possible side effects at the end of the commercial.
Acid blocking medications are the number one selling drugs in the United States accounting for annual sales of more than $13 billion a year. Once only available by prescription they are now available over the counter at your local drug store. With so many people buying drugs to combat stomach acid you would think that it was a horrible thing that we would want to get rid of. Thank goodness we have all of these options, whatever did we do before?
However, there here is another side to this conversation. For the majority of people, the symptoms of heartburn and acid reflux are typically not caused by an over production of stomach acid. In fact, the majority of people suffering from heartburn and reflux actually have low production of stomach acid In addition, suppression of stomach acid can have long[1]term adverse consequences.
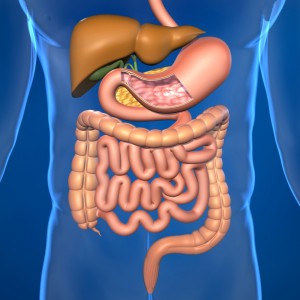
How can this be? Stomach acid is produced by cells that line the stomach. The production is increased in response to food and begins the process of breaking down the meal you just ate. The stomach acid is hydrochloric acid; the same hydrochloric acid that you used in high school chemistry class and that can burn a whole in metal. In order to prevent the acid from burning a hole in the lining of the stomach, the cells that line the stomach produce a layer of mucous that protects the lining and allow the acid to do its job.
When you experience heartburn or reflux some of the stomach acid finds it way up into your esophagus. While your stomach has a nice protective coating, your esophagus does not. So, when the acid accidentally comes up into the esophagus you experience a burning sensation.
At the bottom of the esophagus is a gate called the lower esophageal sphincter (LES). The LES is designed to allow food and liquids to enter the stomach from above, but should prevent the contents of the stomach from coming back up into the esophagus. A number of things can decrease the effectiveness of the LES including smoking, obesity, food allergies, and low stomach acid. When the acid production. is decreased it is more likely for acid to find its way back into your esophagus and cause you pain and discomfort.
Taking an antacid such as Tums, a proton pump inhibitor such as Prilosec, or an H2 blocker such as Zantac do work to decrease the symptoms of heartburn. The proton pump inhibitors are able to suppress stomach acid production by greater than 90%. With very little stomach acid in the stomach there is little chance of the acid finding its way up into the esophagus and so you don’t get reflux or heart burn. The drawback is that you are left without stomach acid.
With low levels of stomach acid you are not able to adequately digest the food that you eat and are more likely to have gastrointestinal issues such as heartburn, reflux, irritable bowel syndrome, diarrhea, constipation, gastritis, gall bladder disease and paradoxically heartburn and reflux. Low stomach acid is also associated with an increase in overgrowth of the small intestine with problematic bacteria. In addition to gastrointestinal dysfunctions, low stomach acid production is also associated with increased risk of numerous disease states outside the gastrointestinal tract including asthma, food Allergies, pneumonia, rheumatoid arthritis (and other autoimmune conditions), depression, rosacea, eczema, anemia.
So next time you are experiencing heartburn, instead of cursing stomach acid and reaching for a pill, think about why you might be having heartburn and work on fixing the underlying cause as opposed to using a treatment that may cause more harm than good. For my tips on preventing heartburn, click here.